To fans of THE 'SCOPE:
We founded THE 'SCOPE back in 2014 as a forum to write about the science behind the news, the culture, and the things that we love. What started out as a venture primarily for family and friends to read quickly blossomed into an enterprise that has amassed hundreds of thousands of readers. We couldn't be happier with the (unexpected) success of the blog and thank everyone for reading and sharing our posts. It has also been a joy to have worked with our fantastic guest contributors over the years.
We're delighted to announce another happy by-product of writing for THE 'SCOPE: it helped land both of us book deals. Based on his popular 'SCOPE series, Mark published The Realization of Star Trek Technologies (Springer) in 2017. Bill's book, Pleased to Meet Me: Genes, Germs, and the Curious Forces That Make Us Who We Are, comes out August 6 on National Geographic Books. We hope you enjoy reading these books as much as we did writing them.
The unhappy consequence is that it took away time we used to have for the blog. We hesitate to close the blog for good, but it is safe to say that posts will less frequent (as you've probably noticed the past year). We have no intention of removing the old posts - they will remain here for your enjoyment.
Here are some other places you can find our writing:
Mark is currently writing at Indiana on Tap, a must-see if you enjoy craft beer.
Bill is blogging at his author website, Psychology Today, and PLOS SciComm. Additional things Bill has written can be found here.
Thanks again for your support over the years! We hope you continue to follow our writing at the sites mentioned above.
Cheers,
Bill Sullivan
Mark Lasbury
Thursday, July 25, 2019
Wednesday, February 6, 2019
Netflix and Cringe: Scientists and Physicians Respond to Goop on Netflix
This week is was announced that Gwyneth Paltrow’s Goop would serve as the basis for a new show on Netflix. Paltrow would co-host the
series, which promises to also "utilize experts, doctors, and researchers to
examine issues relating to physical and spiritual wellness." Goop is the home
of dubious unproven (not to mention expensive) products and advice columns
claiming to enhance health and wellness. Paltrow and her company have
previously been taken to task for promoting unfounded "treatments" such as crystal therapy,
magic stickers, and "Jade Eggs."
There may be some help on the horizon for those concerned about the reckless dissemination of unfounded claims and outright falsehoods. OB/GYN and pain medicine physician, Dr. Jen Gunter, just wrapped production on a new show that promises to provide an antidote against Goop:
Like it or not, Netflix is enabling the spread of Goop. As Goop oozes more into the mainstream, many argue that Netflix should be held accountable for spreading pseudoscientific nonsense that will, at best, have people wasting money, and at worst could be discouraging people from seeking medical care that actually works.
Scientists and medical professionals did not take kindly to
the announcement. Netflix recently raised its subscription price, and many people are miffed
that this revenue is going to support pseudoscience.
Here is a small sampling of recent tweets written in response to the news:
Really? Goop on @Netflix? Are we out of qualified health professionals who provide #credible advice? I know popularity matters but maybe we can make real science popular instead?— Natalia Stasenko, RD (@NataliaStasenko) February 5, 2019
A bleak development. I'm not naive. Money talks. But giving bunk a platform makes the battle for science more difficult. #StreamingThePostModernDarkAge— Timothy Caulfield (@CaulfieldTim) February 5, 2019
And @netflix screws up, badly. https://t.co/ld5B8a0MPm— David Gorski, MD, PhD (@gorskon) February 5, 2019
So more women will be "enlighten" about putting stones in their vaginas and other idiot stuff?!#Netflix #goop pic.twitter.com/MggkPNsEhd— Dr Earth🌍🌎🌏 (@angelovalidiya) February 5, 2019
This sort of shit should be against the law. https://t.co/vskDcumWkC— Dr Siouxsie Wiles (@SiouxsieW) February 5, 2019
There may be some help on the horizon for those concerned about the reckless dissemination of unfounded claims and outright falsehoods. OB/GYN and pain medicine physician, Dr. Jen Gunter, just wrapped production on a new show that promises to provide an antidote against Goop:
It’s ok, she can have her fantasy and fear mongering. I just finished shooting the first season of my fun, factual health show! It will be aspirational vs. authentic— Jennifer Gunter (@DrJenGunter) February 4, 2019
Like it or not, Netflix is enabling the spread of Goop. As Goop oozes more into the mainstream, many argue that Netflix should be held accountable for spreading pseudoscientific nonsense that will, at best, have people wasting money, and at worst could be discouraging people from seeking medical care that actually works.
BILL SULLIVAN is the author of Pleased to Meet Me: How Genes, Germs, and the Environment Make Us Who
We Are (coming August 6, 2019 from National Geographic Books). Sullivan is a professor at the Indiana
University School of Medicine in Indianapolis, where he studies genetics and
infectious disease.
Labels:
Goop,
Gwyneth Paltrow,
health,
medicine,
Netflix,
pseudoscience
Wednesday, November 14, 2018
90 Years Ago, A Contaminated Petri Dish Changed The World
Scientists throw away contaminated petri dishes every day. There is probably a frustrated researcher chucking her petri dishes into the bin right now as you read these words, cursing at the contaminant that ruined her experiment.
In those petri dishes are soft beds of agar that bacteria feast upon. Hundreds of bacterial colonies grow on the agar, each one containing millions of bacterial cells. But fungal spores lurk in the air, and if one of them happens to land on the agar, it may grow better than the bacteria. When a mold appears in a researcher’s bacterial dish, it is not a good thing.
 |
| Alexander Fleming stares menacingly at a plate of bacteria. |
Unless you were keeping your eyes peeled for a substance that can kill bacteria. In the 1920’s, a scientist named Alexander Fleming at St. Mary’s Hospital in London was doing just that. Fleming was growing colonies of Staphylococcus aureus bacteria on his petri dish plates. Staphylococcus aureus is commonly found on the skin, where it normally lives in peace. But it can turn into a deadly troublemaker if it finds its way into the bloodstream. One of Fleming’s first discoveries was that snot could kill the bacteria. He soon isolated the murderous enzyme (lysozyme), but it proved to be a rather weak assassin with no viable therapeutic potential. Besides, it would have been a marketing nightmare...what would you call it? Snoticide? Boogie bombs?
One fateful autumn day in 1928, Fleming arrived at his laboratory to a pile of petri dishes that needed cleaning. While sorting through them, he noticed a mold growing on one of his culture dishes of Staphylococcus aureus. Fleming had undoubtedly seen a contaminated dish of bacteria before, but something more caught his eye that day. It turned out to be the discovery of a lifetime – one that has saved an incalculable number of lives.
As Louis Pasteur said, “Chance favors only the prepared mind.” Fleming’s mind was prepared, and he was always on the lookout for things that could kill bacteria. On that contaminated plate of Staphylococcus aureus, he astutely noted that bacterial colonies grew better if they were farther away from the mold. In fact, no colonies could grow next to the mold. He figured that the mold was producing a substance that was actively killing bacteria that dared to come near it. The miserly mold would want to do this so it could have all the nutrients to itself. Fleming named this mystery bacteria-slaying substance penicillin, since the species of contaminating mold was called Penicillium.
 |
| The famous plate showing bacterial colonies being killed by the mold, Penicillium. |
Fleming published this extraordinary finding in the British Journal of Experimental Pathology in 1929 and the world…paid absolutely no attention to it at all. Pathogenic bacteria continued to lead tens of millions of people to early graves through the 1930’s. Fleming was no chemist, so he was not in position to isolate the active ingredient in the mold that was killing the bacteria. He needed help. But try as he might, Fleming couldn’t get other scientists interested in the promise of mold as a remedy for bacterial infections.
In hindsight, that seems crazy. But there were practical issues that dampened enthusiasm for his idea. At the time, fungi were very difficult to grow in bulk, and the strain of Penicillium Fleming promoted produced very little penicillin. Fleming’s follow-up studies also suggested that penicillin would not work well in the clinic. Because it was so rare, he was forced to use low doses in his attempts to treat ill patients. He also applied the “mold juice” topically on the skin instead of injecting it into the bloodstream, which would have been far more effective. These poorly designed experiments led many to the false conclusion that penicillin was an impotent bacterial assassin. You can imagine the skeptics dismissing his work: “First snot, now mold juice? C’mon, Fleming.” Consequently, Fleming’s discovery laid dormant for over a decade.
In 1939, while leafing through back issues of the British Journal of Experimental Pathology, a chemist at Oxford named Howard Florey decided to revisit Fleming’s ignored penicillin paper. Together with Ernst Boris Chain, this dynamic duo produced a highly purified mold extract and injected it into mice with sepsis. They soon published the striking result that their Penicillium extracts cured the mice of this deadly bacterial infection.
Imagine Fleming’s response when he woke up one day to read this report! Fleming was thrilled that someone was making use of his old work and immediately called Florey to arrange a visit to their laboratory. Chain was surprised to hear that he would get to meet Fleming, as he was under the impression that Fleming had passed away. The trio won the 1945 Nobel Prize in Physiology or Medicine and inspired many microbiologists to search for more bacteria-killing microbes out in the wild. Before long, our medicine cabinet was filled with additional antibiotics like erythromycin, tetracycline, streptomycin, and many more. These wonder drugs were being produced naturally by microbes found in the dirt, on rotting foods, and even in the throat of a chicken. Scientists left no stone unturned in their hunt for weapons of microbial destruction.
 |
| It took ten years before a pair of scientists took Fleming's paper on penicillin seriously. It makes one wonder: How many other medical treasures are buried in obscure scientific journals? |
The story would have a happy ending were it not for two things. In an interview after his Nobel acceptance speech, Fleming gave a very prescient warning about the reckless overuse of antibiotics: "The thoughtless person playing with penicillin treatment is morally responsible for the death of the man who succumbs to infection with the penicillin-resistant organism." Unfortunately, we failed to heed Fleming’s premonition and now face an imminent threat of “superbugs,” bacterial strains that have evolved resistance to these precious medicines. Poor Fleming...ignored twice, but later proven correct on both accounts. Second, virtually no one is in the business of antibiotic discovery anymore because it does not generate high profits like medicines for chronic conditions, which patients must take every day for the rest of their lives. Considered together, Fleming’s near-century old discovery may soon be ineffective and we will return to the “pre-antibiotic” era when a simple scratch from a rosebush could mean death. We need more “prepared minds” in research and in business to keep the antibiotic pipeline strong.
Contributed by: Bill Sullivan
Bill is writing a book! PLEASED TO MEET ME: The Hidden Forces Shaping Who We Are arrives in August 2019 from National Geographic Books.
Labels:
antibiotics,
bacteria,
drugs,
Fleming,
medicine,
microbiology,
penicillin
Wednesday, July 18, 2018
If Parasites Had Dating Profiles
Once upon a time, before the Internet, people actually had
to venture outside to find a significant other. Popular places to find a
potential mate included bars, dance clubs, dog parks, cafes, parties, and the
gym. You’d have to work up the courage, and perhaps a cringe-worthy pick-up
line, to ask another person out on a date. After an overpriced dinner and
movie, you’d have to engage in lengthy conversation under a starry sky to learn
about them.
But who has time for all that?! These days, you can simply screen dozens of candidates by reading their dating profiles on matchmaking web sites or apps like Tinder. This modern form of mate selection is unique to humans; imagine if other creatures in the natural world, like parasites, had to write dating profiles…
Toxoplasma gondii
When I get into something that is not a cat, I get bored rather quickly and go to sleep. You can call me bradyzoite when I’m napping. Life in my intermediate host isn’t all that bad. I can pick pretty much whatever cell type I want and make it my room. The neurons in the brain are ideal because the pesky immune system tends to leave that organ alone, so I get plenty of peace and quiet. I just chill and wait for that animal to get eaten, hopefully by a cat so I can get my groove on again! What if another type of animal eats me instead? No biggie. I’m a patient parasite and will simply wait it out in another intermediate host.
Like I said before, if I landed in a rodent I know how to scramble their tiny brains to increase their chances of getting eaten by a hairball-coughing feline. The human brain is a tad more complex and taking me a little longer to figure out. While knocking around in a human head, I might have increased the risk of some people to develop schizophrenia or rage disorder. But ultimately, I’m trying to rewire the human brain so they leap into lion cages at the zoo.
In my spare time, I love to devour books instead of organ meat. My favorite books include Cat’s Cradle, The Pink Panther, The White Tiger, and of course The Cat in the Hat. I’m also writing my own book. It’s called If You Give A Mouse Toxoplasma…
I think you’ll be surprised how easy it is to burrow into a human's skin – I prefer to enter through a hair follicle. They don’t feel a thing. Once we get inside a human, we can ditch our tails and I’ll give you a grand tour. After a few days gallivanting through the skin, we’ll hang out in the lungs, go through the heart, and then enjoy a bloodmeal as we take a ride in the circulatory system to the liver. This is the stop I find most arousing, and I’ll ask you to pair-bond with me. If you accept, we’ll celebrate by making our way to the veins draining the colon.
Why the veins of the colon? I’m glad you asked, my pet! You see, the colon is where the human stores his waste until he can’t hold it in any longer. We can easily send our eggs into his colon, giving our kids a free ride back out into the water so they can find snails of their own one day. It’s a strategy not unlike the one used by Han Solo in The Empire Strikes Back when he evaded the Star Destroyer by making it appear his ship was just a part of the Imperial garbage.
I think you’ll find that the chemistry between us is no fluke, but rather truly meant to be.
What could be more romantic than a date that involves a
“kissing” bug? That is where our enchanting evening shall begin. From inside
the so-called kissing bug, we will watch it latch onto human flesh and suck its
blood – cool, huh? After the kissing bug has its fill, it gets the urge to go
to the bathroom, using the tiny wound it made as a toilet. That will be our cue
to exit: out of the kissing bug, into the human – right through that convenient little
hole the bug made in its flesh.
Once under the human’s skin, we’ll transform from trypomastigotes into amastigotes while inside the host’s cells. I hope you don’t think I’m being too prudish, but I’m really not all that into sex. I’d prefer that we multiply on our own, but how about this…we can watch each other divide!
After we make clones of ourselves, there will be too many for the host cell to hold. I just love it when a host cell pops, don’t you? As trypomastigotes again, we’ll be free floating in the blood, where we will hitch a ride when the next hungry bug comes along to “kiss” our human host.
I just hope the kids we leave behind don’t cause trouble. Most of the time when I go through a human, my kids get all rowdy and start having a bunch of kids of their own. The extensive damage they leave in their wake can cause serious problems for the human host, which they call Chagas disease.
While waiting for a kissing bug to pick me up, I enjoy listening to music. Some of my favorite songs include Kiss Me Deadly, Love Bites, and Blow Me (One Last Kiss).
The mosquito will be our limo to a fine human restaurant where the blood flows like wine. We will get our wake-up call when the mosquito bites a person; then hang tight while we take an exhilarating slide down her proboscis and into a red river. After a quick pit stop in the liver to transform into merozoites and put on our bibs, we’ll jump back into the red river and take our pick at which blood cell we’d like to dine at first. All the hemoglobin you can eat! We will be the envy of Count Dracula!
In humans, red blood cells carry oxygen around the body, so as we destroy them, our human host will soon feel woozy, suffering from anemia, chills, and fever. But have no fear, as I’ll send out an SOS that changes our victim’s scent to be more attractive to mosquitoes. Before you know it, we’ll be pulled up into a fresh mosquito for some more amore.
I’m also a huge movie buff. My favorite movies are The Mosquito Coast, There Will Be Blood, Jungle Fever, and Red River.
But who has time for all that?! These days, you can simply screen dozens of candidates by reading their dating profiles on matchmaking web sites or apps like Tinder. This modern form of mate selection is unique to humans; imagine if other creatures in the natural world, like parasites, had to write dating profiles…
Toxoplasma gondii
 |
Hanging with my BFFs in a tissue cyst.
We call ourselves "The Brady Bunch"!
Photo by David Ferguson (via EurekAlert)
|
Do you love cats? So do I! They’re my favorite animal,
although I can weasel my way into any vertebrate animal that I want to,
including weasels. That’s one of the reasons why I’m called “the most
successful parasite on Earth.” I’m the clever parasite that has learned to
manipulate the brains of rodents so that they become fearless morons around
felines. Normally, mice and rats scurry away from the scent of a cat, but not
when I’m in their head!
What turns me on? Long, romantic walks through the hollows
of a cat’s innards. I like to groove under the moist sheets of their intestinal
epithelium to the musical stylings of Cat Stevens. If we have kids, I promise
to be a good parent and read Calvin and
Hobbes to them all night long. I’ll be sure to kiss them goodbye before
sending them out into the world to contaminate litter boxes, sandboxes,
gardens, yards, and streams. Before long, our progeny will be inhaled or
ingested by unsuspecting animals.When I get into something that is not a cat, I get bored rather quickly and go to sleep. You can call me bradyzoite when I’m napping. Life in my intermediate host isn’t all that bad. I can pick pretty much whatever cell type I want and make it my room. The neurons in the brain are ideal because the pesky immune system tends to leave that organ alone, so I get plenty of peace and quiet. I just chill and wait for that animal to get eaten, hopefully by a cat so I can get my groove on again! What if another type of animal eats me instead? No biggie. I’m a patient parasite and will simply wait it out in another intermediate host.
Like I said before, if I landed in a rodent I know how to scramble their tiny brains to increase their chances of getting eaten by a hairball-coughing feline. The human brain is a tad more complex and taking me a little longer to figure out. While knocking around in a human head, I might have increased the risk of some people to develop schizophrenia or rage disorder. But ultimately, I’m trying to rewire the human brain so they leap into lion cages at the zoo.
In my spare time, I love to devour books instead of organ meat. My favorite books include Cat’s Cradle, The Pink Panther, The White Tiger, and of course The Cat in the Hat. I’m also writing my own book. It’s called If You Give A Mouse Toxoplasma…
Schistosoma mansoni
 |
Come swim with Schisto!
Photo: http://schaechter.asmblog.org/.a/
6a00d8341c5e1453ef014e875d2f3e970d-popup
|
Escargot, anyone? My name is Schistosoma, but you can call
me Schisto. I live in parts of South America and the Caribbean, Africa, and the
Middle East. I hope you don’t think I’m being too fresh, but I’d love to start
our date by skinny dipping in my favorite freshwater lake. After we’re done
frolicking in the water, we’ll sneak into some snails and develop into cercariae.
What? You’ve never been a cercariae before? Have no fear, my darling, I will
teach you how to become one. Once we’re cercariae, we’ll break out of the snail
and search for the definitive stop on our romantic adventure: an unsuspecting
human swimming in our waters.
The cool thing about becoming cercariae is that we’ll look
like a mermaid. We’ll gain a gorgeous forked tail that will help us swim around
and find a suitable human to invade. I like to hum the theme to Jaws as I make
my approach to the human creature! Do you know how many people are attacked by sharks each year? Only 75. I've infected well over 200 million people, but sharks get the scary theme song...go figure!I think you’ll be surprised how easy it is to burrow into a human's skin – I prefer to enter through a hair follicle. They don’t feel a thing. Once we get inside a human, we can ditch our tails and I’ll give you a grand tour. After a few days gallivanting through the skin, we’ll hang out in the lungs, go through the heart, and then enjoy a bloodmeal as we take a ride in the circulatory system to the liver. This is the stop I find most arousing, and I’ll ask you to pair-bond with me. If you accept, we’ll celebrate by making our way to the veins draining the colon.
Why the veins of the colon? I’m glad you asked, my pet! You see, the colon is where the human stores his waste until he can’t hold it in any longer. We can easily send our eggs into his colon, giving our kids a free ride back out into the water so they can find snails of their own one day. It’s a strategy not unlike the one used by Han Solo in The Empire Strikes Back when he evaded the Star Destroyer by making it appear his ship was just a part of the Imperial garbage.
I think you’ll find that the chemistry between us is no fluke, but rather truly meant to be.
Trypanosoma cruzi
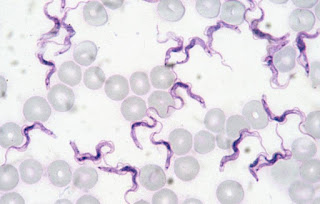 |
Come cruzi with me! I'm the cute wavy purple things!
Photo: Wikipedia Commons
|
Once under the human’s skin, we’ll transform from trypomastigotes into amastigotes while inside the host’s cells. I hope you don’t think I’m being too prudish, but I’m really not all that into sex. I’d prefer that we multiply on our own, but how about this…we can watch each other divide!
After we make clones of ourselves, there will be too many for the host cell to hold. I just love it when a host cell pops, don’t you? As trypomastigotes again, we’ll be free floating in the blood, where we will hitch a ride when the next hungry bug comes along to “kiss” our human host.
I just hope the kids we leave behind don’t cause trouble. Most of the time when I go through a human, my kids get all rowdy and start having a bunch of kids of their own. The extensive damage they leave in their wake can cause serious problems for the human host, which they call Chagas disease.
While waiting for a kissing bug to pick me up, I enjoy listening to music. Some of my favorite songs include Kiss Me Deadly, Love Bites, and Blow Me (One Last Kiss).
Plasmodium falciparum
 |
I'm a little camera shy, but I like these plushies of me
as they show my softer side!
Photo: Giant Microbes
|
If you have a fetish for vampires or other blood-sucking
creatures, I am the parasite for you! My name is Plasmodium, but most people know me as malaria, which means “bad
air.” I hasten to clarify: I do not suffer from flatulence or rancid breath.
Before people realized I was a parasite, they attributed the cause of malaria
to breathing in “bad air.”
Two of my favorite things in life are blood and sex. I use
humans for blood and Anopheles
mosquitoes for sex. You might not think that there is enough room in the gut of
a mosquito to have a lot of great sex, but give me a chance and I’ll show you
that size isn’t everything. After the love making, we’ll take a lovely stroll
up to the mosquito’s salivary glands and take a little nap before dinner. While
we’re in the salivary glands, you can call me sporozoite.The mosquito will be our limo to a fine human restaurant where the blood flows like wine. We will get our wake-up call when the mosquito bites a person; then hang tight while we take an exhilarating slide down her proboscis and into a red river. After a quick pit stop in the liver to transform into merozoites and put on our bibs, we’ll jump back into the red river and take our pick at which blood cell we’d like to dine at first. All the hemoglobin you can eat! We will be the envy of Count Dracula!
In humans, red blood cells carry oxygen around the body, so as we destroy them, our human host will soon feel woozy, suffering from anemia, chills, and fever. But have no fear, as I’ll send out an SOS that changes our victim’s scent to be more attractive to mosquitoes. Before you know it, we’ll be pulled up into a fresh mosquito for some more amore.
I’m also a huge movie buff. My favorite movies are The Mosquito Coast, There Will Be Blood, Jungle Fever, and Red River.
Contributed by: Bill Sullivan
Follow Bill on Twitter.
Labels:
love,
malaria,
microbiology,
parasites,
Schistosomes,
Toxoplasma,
Trypanosoma
Friday, February 16, 2018
Can Your Cat Cause Demonic Possession?

Cats are routinely associated with malevolent entities in horror
stories. They are the favorite pet of witches and villains, a frequent denizen
of haunted houses, and the object of several superstitions. Now doctors have
linked felines to demonic possession!
Wait, what?
In a new case study published yesterday in the journal Medicine, scientists in China reported that acute infection with the common parasite Toxoplasma gondii triggered the onset of an unusual autoimmune disease called anti-N-methyl-D-aspartate (NMDA) receptor encephalitis. Anti-NMDA receptor encephalitis occurs when the body attacks one of its own brain proteins, leading to bizarre personality changes that mimic the stereotypical behaviors that come to mind when we think about demonic possession.
In this case report, a nine-year-old girl arrived at the hospital with seizures, headache, and vomiting. Then she developed unexplained personality and behavior changes. She tested positive for both anti-NMDA receptor antibodies and recent infection with the Toxoplasma parasite.
Anti-NMDA receptor encephalitis was the subject of the bestselling book, Brain on Fire: My Month of Madness, by Susannah Cahalan. In this memoir, which reads like an episode of Mystery Diagnosis, Cahalan describes her terrifying transformation from a vibrant young journalist to an unrecognizable and violent monster. As her condition progressed, she grew paranoid of others, thought family members were imposters, and lashed out at people. She lost control of her bodily movements, suffered seizures, and spoke in tongues. If you didn’t know better, you’d claim she needed an exorcist. Luckily, a neurologist properly diagnosed her disease and gave her immune suppressant drugs that drove it into remission.
Wait, what?
In a new case study published yesterday in the journal Medicine, scientists in China reported that acute infection with the common parasite Toxoplasma gondii triggered the onset of an unusual autoimmune disease called anti-N-methyl-D-aspartate (NMDA) receptor encephalitis. Anti-NMDA receptor encephalitis occurs when the body attacks one of its own brain proteins, leading to bizarre personality changes that mimic the stereotypical behaviors that come to mind when we think about demonic possession.
In this case report, a nine-year-old girl arrived at the hospital with seizures, headache, and vomiting. Then she developed unexplained personality and behavior changes. She tested positive for both anti-NMDA receptor antibodies and recent infection with the Toxoplasma parasite.
Anti-NMDA receptor encephalitis was the subject of the bestselling book, Brain on Fire: My Month of Madness, by Susannah Cahalan. In this memoir, which reads like an episode of Mystery Diagnosis, Cahalan describes her terrifying transformation from a vibrant young journalist to an unrecognizable and violent monster. As her condition progressed, she grew paranoid of others, thought family members were imposters, and lashed out at people. She lost control of her bodily movements, suffered seizures, and spoke in tongues. If you didn’t know better, you’d claim she needed an exorcist. Luckily, a neurologist properly diagnosed her disease and gave her immune suppressant drugs that drove it into remission.
 |
| Did Regan have a cat? |
It is not clear why some people (mostly women) start making
antibodies that attack the NMDA receptors in their brain. Some cases are linked
to the development of tumors, especially teratomas in the ovaries. Certain
viruses that infect the brain, including herpes simplex virus, have also been
linked to anti-NMDA receptor encephalitis. Now it seems Toxoplasma, which also infects the brain, may be a trigger of this
haunting disease, too.
Toxoplasma is a devious parasite with a complex life cycle. It is capable of infecting any warm-blooded animal, but can only complete its sexual cycle in the intestines of cats. After infecting a cat, the cat spews billions of infectious parasite oocysts into the litter box (or the environment) for up to two weeks. These oocysts are very sturdy and can last up to two years in the environment, giving them plenty of time to be inhaled or ingested by another animal (including humans). In addition to picking up oocysts from the litter box, garden, or sandbox, we can also acquire the infection by eating undercooked meat or unwashed fruits and vegetables.
Once a person becomes infected, the parasite disseminates throughout bodily tissues, including the brain and heart, and transitions into a latent stage called the tissue cyst. While current treatments can stop the parasite from replicating, no drug exists that can get rid of the tissue cysts. In other words, infection with Toxoplasma is permanent. The thought of having a brain filled with these parasites is disquieting, but most scientists believe the cysts are inert unless the individual becomes immune compromised, in which case the parasites can cause massive tissue damage from unchecked growth.
A growing number of scientists argue, however, that in certain individuals the Toxoplasma tissue cysts are not benign and may cause neurological disorders. One of the better-established correlations is the link between Toxoplasma infection and schizophrenia. Interestingly, up to 10% of schizophrenia patients test positive for anti-NMDA receptor antibodies.
The mechanism explaining how Toxoplasma infection may cause anti-NMDA receptor encephalitis remains to be elucidated. Toxoplasma infection is remarkably common (up to one-third of the global population is believed to carry this parasite), but anti-NMDA receptor encephalitis is rare. For now, the authors of the study advise that clinicians assess the possibility of Toxoplasma infection when evaluating a patient with anti-NMDA receptor encephalitis.
To prevent Toxoplasma infection and minimize your chances of becoming possessed by this parasite, be sure to thoroughly cook meat and wash produce and veggies. Wear gloves and a mask when gardening and keep sandboxes covered when not in use. You cannot catch Toxoplasma by petting your cat, but it is important to clean the litter box promptly and wash your hands with soap and water. Pregnant women, in particular, should heed these warnings as infection during pregnancy can lead to miscarriage or serious congenital birth defects. See the infographic below for more.
UPDATE (7/26/18): A new study was published today by Li et al. that used a mouse model of infection to show that anti-NMDA receptor autoantibodies are induced by the presence of latent Toxoplasma tissue cysts.
Brain on Fire has also been made into a movie that can be seen now on Netflix.
Toxoplasma is a devious parasite with a complex life cycle. It is capable of infecting any warm-blooded animal, but can only complete its sexual cycle in the intestines of cats. After infecting a cat, the cat spews billions of infectious parasite oocysts into the litter box (or the environment) for up to two weeks. These oocysts are very sturdy and can last up to two years in the environment, giving them plenty of time to be inhaled or ingested by another animal (including humans). In addition to picking up oocysts from the litter box, garden, or sandbox, we can also acquire the infection by eating undercooked meat or unwashed fruits and vegetables.
Once a person becomes infected, the parasite disseminates throughout bodily tissues, including the brain and heart, and transitions into a latent stage called the tissue cyst. While current treatments can stop the parasite from replicating, no drug exists that can get rid of the tissue cysts. In other words, infection with Toxoplasma is permanent. The thought of having a brain filled with these parasites is disquieting, but most scientists believe the cysts are inert unless the individual becomes immune compromised, in which case the parasites can cause massive tissue damage from unchecked growth.
A growing number of scientists argue, however, that in certain individuals the Toxoplasma tissue cysts are not benign and may cause neurological disorders. One of the better-established correlations is the link between Toxoplasma infection and schizophrenia. Interestingly, up to 10% of schizophrenia patients test positive for anti-NMDA receptor antibodies.
The mechanism explaining how Toxoplasma infection may cause anti-NMDA receptor encephalitis remains to be elucidated. Toxoplasma infection is remarkably common (up to one-third of the global population is believed to carry this parasite), but anti-NMDA receptor encephalitis is rare. For now, the authors of the study advise that clinicians assess the possibility of Toxoplasma infection when evaluating a patient with anti-NMDA receptor encephalitis.
To prevent Toxoplasma infection and minimize your chances of becoming possessed by this parasite, be sure to thoroughly cook meat and wash produce and veggies. Wear gloves and a mask when gardening and keep sandboxes covered when not in use. You cannot catch Toxoplasma by petting your cat, but it is important to clean the litter box promptly and wash your hands with soap and water. Pregnant women, in particular, should heed these warnings as infection during pregnancy can lead to miscarriage or serious congenital birth defects. See the infographic below for more.
UPDATE (7/26/18): A new study was published today by Li et al. that used a mouse model of infection to show that anti-NMDA receptor autoantibodies are induced by the presence of latent Toxoplasma tissue cysts.
Brain on Fire has also been made into a movie that can be seen now on Netflix.
Contributed by: Bill Sullivan
Labels:
cancer,
cats,
demons,
immunology,
infectious disease,
medicine,
parasites,
Toxoplasma
Monday, November 27, 2017
Biohacking and DIY Gene Therapy: Revolution or Hi-tech Snake Oil?
Do you want bigger muscles? Want to make those brown eyes
blue? Does your memory resemble a slice of Swiss cheese? Well, step right up
and let me tell you about biohacking! Lend me your ears…and I’ll tell you how
to improve them! With our new do-it-yourself genetic engineering kits, you can
change whatever genes you want!
Bio-savvy entrepreneurs are determined to make biohacking a
mainstream activity. Companies
are emerging that promote DIY gene therapy, so now anyone with an opposable
thumb can pipet DNA changes into their bodies, their pesky little sister, pets,
or just about any living creature they encounter.
 |
| Wouldn’t you like to be a biohacker too? Or is biohacking just the latest incarnation of snake oil? |
Those products seem benign compared to Zayner’s ultimate
objective: selling genetic engineering tools to the masses so they can modify
their own genes, or those of other living creatures, in whatever way they want
without any oversight or regulatory approval. Zayner has already initiated
experiments on himself and encourages others to join him on this wild ride. In
the rambling presentation below, Zayner explains over shots of scotch and F-bombs
that he wants to crowdsource genetic engineering because he believes it will
facilitate innovation. Why let professional scientists have all the fun? Zayner
demonstrated how easy biohacking your genome can be by injecting the reagents
into his arm during the presentation and distributing free samples for the
audience to take home.
Let’s take a closer look at his idea. Zayner is using CRISPR/Cas9,
a powerful new tool for gene editing, to disable his myostatin gene (learn about
the basics
of CRISPR/Cas9 and its application
in gene therapy). Cas9 is a DNA-cutting enzyme that is directed to a
specific site in DNA by a guide sequence. Myostatin stops muscles from growing,
so his plan is to knockout this gene in his muscle cells in hopes that it will
make them grow once again. Given his affinity for scotch, a more useful
experiment might have been to enhance his alcohol dehydrogenase genes.
There is evidence linking the depletion of myostatin to
muscle growth. Mice
engineered to lack myostatin have double their normal skeletal muscle mass.
CRISPR/Cas9 has been specifically used to knockout myostatin in animal embryos,
such as rabbits, and the
genetically modified animals grew to have more muscle mass. Moreover, when
humans are born with mutations that lead to less functional myostatin, they
also have more muscle mass (or, in less pleasant-sounding medical terms, “gross muscle
hypertrophy”).
CRISPR has already been used to successfully modify human
embryos (none were implanted), but to date, no one has tried CRISPR/Cas9 in a
living adult. Zayner’s strategy is to simply inject plasmid DNA that contains the
Cas9 gene along with the guide sequence that directs it to the myostatin gene.
Importantly, he’s produced no evidence yet to show that these reagents work in human cells. Ideally, we’d like to see confirmation of the gene modification in a muscle biopsy from Zayner, or proof that his approach works in an adult animal model. At the very least, it would be useful to know whether his system alters the gene in cultured cells.
Importantly, he’s produced no evidence yet to show that these reagents work in human cells. Ideally, we’d like to see confirmation of the gene modification in a muscle biopsy from Zayner, or proof that his approach works in an adult animal model. At the very least, it would be useful to know whether his system alters the gene in cultured cells.
So, can this really work? There are some formidable
obstacles and shortcomings. First, the injected plasmid DNA has to get into the
muscle cells. Many would argue that the DNA is likely to be degraded or damaged
along the way. There is scarce evidence that intramuscular injection of DNA
works, but I did find one
study done in mice from 1993 suggesting it is possible, although expression
levels of the gene injected in this mouse study varied. Variations in the
levels of Cas9 or the guide sequence would certainly affect the outcome.
Nevertheless, let’s pretend some of it gets into a few muscle cells and they make the Cas9 protein and its guide sequence. The next big assumption we have to make is that the guide sequence used actually cuts the myostatin gene. Multiple guide sequences usually have to be tried to find one that works and, as mentioned above, I’ve seen no evidence that this particular guide sequence operates as it should in human cells.
Additionally, you have two copies (alleles) of myostatin,
one from mom and one from dad. To knockout myostatin completely, Cas9 would
have to cut both alleles. Let’s assume we get that far and both alleles of
myostatin are cut. Sometimes cells can repair the DNA cut without incident. For
myostatin to be disabled, the cell would have to make a mistake when repairing
the severed DNA (which they do, but not all the time). Assuming we jump all
these hurdles, that one cell or handful of cells is not likely to produce any
noticeable change in muscle mass, especially if only one allele was disabled.
Zayner claims repeated injections might overcome this issue, but given the
sheer number of cells that would need to be altered to produce a visible
effect, the claim seems to be on very shaky ground.
Despite all the caveats, disrupting a gene is actually the
easiest application of CRISPR/Cas9. To add or change a genetic sequence, an
additional fragment of DNA needs to be incorporated where Cas9 made the incision.
And if you wanted to use CRISPR/Cas9 to give yourself wings or eyes in the back
of your head, you can forget about that. We are nowhere close to knowing how to
do such things.
More alarming, there is risk of dangerous side-effects. While the loss of myostatin will increase muscle size as well as bone mineral density and bone mass, it also leads to spinal disc degeneration and spinal osteoarthritis. Second, there is a risk of infection or an allergic reaction to the injections. Third, CRISPR/Cas9 has been reported to produce so-called “off-target” effects. In other words, the guide sequence sometimes escorts Cas9 to other places in the genome, where it may introduce cuts in genes that were not intended to be destroyed—a genetic equivalent of friendly fire.
There’s also the possibility that the CRISPR/Cas9 plasmid itself
could integrate into the genome, again possibly disrupting critical genes. One study showed that DNA
injected into mouse muscles persisted for life, cranking out the protein
constantly. What would happen if Cas9 continues to be produced in Zayner’s
cells for the rest of his life? In the worst-case scenario, it would continue
to cut up his DNA indiscriminately. There’s also a study in mice suggesting
that DNA injection can
accelerate autoimmune responses. Finally, unlike injecting an embryo in
which all cells have a high probability of being modified, Zayner’s approach is
going to produce mosaic effects. In other words, some cells will be edited, but
others will not, which could result in a disfigured arm. Zayner dismisses all of these risks with disquieting nonchalance.
 |
| If you don’t want to risk modifying your genome to kill your myostatin gene, you can always buy inflatable muscles to wear under your shirt. |
There’s no product currently available from The ODIN that could bring on the apocalypse, but it is the principle that concerns many people, scientists and non-scientists alike. Even the most avid science enthusiasts are likely to take issue with providing potential crackpots the tools to screw with the recipe of life. Genetic engineering is exciting and promising, but must be explored with great caution by well-trained professionals following reasonable regulations because there is no way to unscramble this egg.
 |
| Biohacking has been banned in several countries, and on November 21, 2017 the FDA updated their web site to state that self-administration of gene therapy is against the law. It seems that Zayner, a self-professed fan of the TV show Survivor, just had his torch snuffed out by government regulators chanting, “The tribe has spoken.” |
Contributed by: Bill
Sullivan
Follow Bill on
Twitter.
The author thanks Colin Sullivan for research assistance and helpful discussions, and Jason Organ for editing and helpful suggestions.
The author thanks Colin Sullivan for research assistance and helpful discussions, and Jason Organ for editing and helpful suggestions.
Subscribe to:
Posts (Atom)
