Cats are routinely associated with malevolent entities in horror
stories. They are the favorite pet of witches and villains, a frequent denizen
of haunted houses, and the object of several superstitions. Now doctors have
linked felines to demonic possession!
Wait, what?
In a new case study published yesterday in the journal Medicine, scientists in China reported that acute infection with the common parasite Toxoplasma gondii triggered the onset of an unusual autoimmune disease called anti-N-methyl-D-aspartate (NMDA) receptor encephalitis. Anti-NMDA receptor encephalitis occurs when the body attacks one of its own brain proteins, leading to bizarre personality changes that mimic the stereotypical behaviors that come to mind when we think about demonic possession.
In this case report, a nine-year-old girl arrived at the hospital with seizures, headache, and vomiting. Then she developed unexplained personality and behavior changes. She tested positive for both anti-NMDA receptor antibodies and recent infection with the Toxoplasma parasite.
Anti-NMDA receptor encephalitis was the subject of the bestselling book, Brain on Fire: My Month of Madness, by Susannah Cahalan. In this memoir, which reads like an episode of Mystery Diagnosis, Cahalan describes her terrifying transformation from a vibrant young journalist to an unrecognizable and violent monster. As her condition progressed, she grew paranoid of others, thought family members were imposters, and lashed out at people. She lost control of her bodily movements, suffered seizures, and spoke in tongues. If you didn’t know better, you’d claim she needed an exorcist. Luckily, a neurologist properly diagnosed her disease and gave her immune suppressant drugs that drove it into remission.
Wait, what?
In a new case study published yesterday in the journal Medicine, scientists in China reported that acute infection with the common parasite Toxoplasma gondii triggered the onset of an unusual autoimmune disease called anti-N-methyl-D-aspartate (NMDA) receptor encephalitis. Anti-NMDA receptor encephalitis occurs when the body attacks one of its own brain proteins, leading to bizarre personality changes that mimic the stereotypical behaviors that come to mind when we think about demonic possession.
In this case report, a nine-year-old girl arrived at the hospital with seizures, headache, and vomiting. Then she developed unexplained personality and behavior changes. She tested positive for both anti-NMDA receptor antibodies and recent infection with the Toxoplasma parasite.
Anti-NMDA receptor encephalitis was the subject of the bestselling book, Brain on Fire: My Month of Madness, by Susannah Cahalan. In this memoir, which reads like an episode of Mystery Diagnosis, Cahalan describes her terrifying transformation from a vibrant young journalist to an unrecognizable and violent monster. As her condition progressed, she grew paranoid of others, thought family members were imposters, and lashed out at people. She lost control of her bodily movements, suffered seizures, and spoke in tongues. If you didn’t know better, you’d claim she needed an exorcist. Luckily, a neurologist properly diagnosed her disease and gave her immune suppressant drugs that drove it into remission.
 |
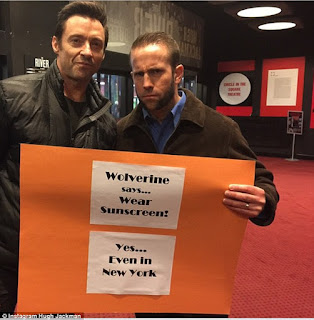
| Did Regan have a cat? |
It is not clear why some people (mostly women) start making
antibodies that attack the NMDA receptors in their brain. Some cases are linked
to the development of tumors, especially teratomas in the ovaries. Certain
viruses that infect the brain, including herpes simplex virus, have also been
linked to anti-NMDA receptor encephalitis. Now it seems Toxoplasma, which also infects the brain, may be a trigger of this
haunting disease, too.
Toxoplasma is a devious parasite with a complex life cycle. It is capable of infecting any warm-blooded animal, but can only complete its sexual cycle in the intestines of cats. After infecting a cat, the cat spews billions of infectious parasite oocysts into the litter box (or the environment) for up to two weeks. These oocysts are very sturdy and can last up to two years in the environment, giving them plenty of time to be inhaled or ingested by another animal (including humans). In addition to picking up oocysts from the litter box, garden, or sandbox, we can also acquire the infection by eating undercooked meat or unwashed fruits and vegetables.
Once a person becomes infected, the parasite disseminates throughout bodily tissues, including the brain and heart, and transitions into a latent stage called the tissue cyst. While current treatments can stop the parasite from replicating, no drug exists that can get rid of the tissue cysts. In other words, infection with Toxoplasma is permanent. The thought of having a brain filled with these parasites is disquieting, but most scientists believe the cysts are inert unless the individual becomes immune compromised, in which case the parasites can cause massive tissue damage from unchecked growth.
A growing number of scientists argue, however, that in certain individuals the Toxoplasma tissue cysts are not benign and may cause neurological disorders. One of the better-established correlations is the link between Toxoplasma infection and schizophrenia. Interestingly, up to 10% of schizophrenia patients test positive for anti-NMDA receptor antibodies.
The mechanism explaining how Toxoplasma infection may cause anti-NMDA receptor encephalitis remains to be elucidated. Toxoplasma infection is remarkably common (up to one-third of the global population is believed to carry this parasite), but anti-NMDA receptor encephalitis is rare. For now, the authors of the study advise that clinicians assess the possibility of Toxoplasma infection when evaluating a patient with anti-NMDA receptor encephalitis.
To prevent Toxoplasma infection and minimize your chances of becoming possessed by this parasite, be sure to thoroughly cook meat and wash produce and veggies. Wear gloves and a mask when gardening and keep sandboxes covered when not in use. You cannot catch Toxoplasma by petting your cat, but it is important to clean the litter box promptly and wash your hands with soap and water. Pregnant women, in particular, should heed these warnings as infection during pregnancy can lead to miscarriage or serious congenital birth defects. See the infographic below for more.
UPDATE (7/26/18): A new study was published today by Li et al. that used a mouse model of infection to show that anti-NMDA receptor autoantibodies are induced by the presence of latent Toxoplasma tissue cysts.
Brain on Fire has also been made into a movie that can be seen now on Netflix.
Toxoplasma is a devious parasite with a complex life cycle. It is capable of infecting any warm-blooded animal, but can only complete its sexual cycle in the intestines of cats. After infecting a cat, the cat spews billions of infectious parasite oocysts into the litter box (or the environment) for up to two weeks. These oocysts are very sturdy and can last up to two years in the environment, giving them plenty of time to be inhaled or ingested by another animal (including humans). In addition to picking up oocysts from the litter box, garden, or sandbox, we can also acquire the infection by eating undercooked meat or unwashed fruits and vegetables.
Once a person becomes infected, the parasite disseminates throughout bodily tissues, including the brain and heart, and transitions into a latent stage called the tissue cyst. While current treatments can stop the parasite from replicating, no drug exists that can get rid of the tissue cysts. In other words, infection with Toxoplasma is permanent. The thought of having a brain filled with these parasites is disquieting, but most scientists believe the cysts are inert unless the individual becomes immune compromised, in which case the parasites can cause massive tissue damage from unchecked growth.
A growing number of scientists argue, however, that in certain individuals the Toxoplasma tissue cysts are not benign and may cause neurological disorders. One of the better-established correlations is the link between Toxoplasma infection and schizophrenia. Interestingly, up to 10% of schizophrenia patients test positive for anti-NMDA receptor antibodies.
The mechanism explaining how Toxoplasma infection may cause anti-NMDA receptor encephalitis remains to be elucidated. Toxoplasma infection is remarkably common (up to one-third of the global population is believed to carry this parasite), but anti-NMDA receptor encephalitis is rare. For now, the authors of the study advise that clinicians assess the possibility of Toxoplasma infection when evaluating a patient with anti-NMDA receptor encephalitis.
To prevent Toxoplasma infection and minimize your chances of becoming possessed by this parasite, be sure to thoroughly cook meat and wash produce and veggies. Wear gloves and a mask when gardening and keep sandboxes covered when not in use. You cannot catch Toxoplasma by petting your cat, but it is important to clean the litter box promptly and wash your hands with soap and water. Pregnant women, in particular, should heed these warnings as infection during pregnancy can lead to miscarriage or serious congenital birth defects. See the infographic below for more.
UPDATE (7/26/18): A new study was published today by Li et al. that used a mouse model of infection to show that anti-NMDA receptor autoantibodies are induced by the presence of latent Toxoplasma tissue cysts.
Brain on Fire has also been made into a movie that can be seen now on Netflix.
Contributed by: Bill Sullivan